
What happens when a medication once hailed as a lifesaver becomes outdated? Blood pressure drugs aren’t immune to this shift, either. Doctors are now phasing out certain medications due to side effects or newer alternatives. Here’s a closer look at ten medications that are becoming less common on pharmacy shelves.
Alpha-Blockers
Alpha-blockers once gained traction for hypertension due to their ability to relax blood vessels. Despite initial success, doctors noticed they were linked to heart failure risks, which prompted them to reconsider administering these medications. Today, their use has shifted to managing prostate conditions rather than routine pressure control.
Beta-Blockers
While they are no longer preferred as the first-line for treating primary high blood pressure, beta-blockers remain vital for managing specific heart conditions such as atrial fibrillation or coronary artery disease. Their use is now more condition-specific, and they are also used as add-ons for treatment.
Peripheral Vasodilators
Peripheral vasodilators provided direct vessel relaxation, effectively lowering blood pressure. However, side effects like fluid retention and tachycardia have reduced their therapeutic value. Today, more targeted vasodilators deliver consistent results, and older versions are used less often, primarily in specific clinical scenarios.
Central Alpha Agonists
Originally used as a primary option for resistant cases, central alpha agonists saw reduced use due to sedative effects and rebound risks. But now, they are used only in specific cases and serve as secondary treatments for high blood pressure when standard therapies don’t work.
Short-Acting Calcium Channel Blockers

Short-acting calcium channel blockers initially gained attention for their quick hypertension-reduction effects. However, they later raised concerns due to abrupt drops in blood pressure levels and increased cardiac risk. Extended-release versions now take precedence, with short-acting forms reserved for closely monitored clinical scenarios.
Potassium Channel Openers

Minoxidil and Diazoxide, both potassium channel openers, once managed severe hypertension by relaxing blood vessels and reducing vascular resistance. Severe side effects, including fluid retention and excessive hair growth, limited their use. Doctors preferred the adoption of safer, more targeted antihypertensive medications.
Direct Renin Inhibitors

Introduced as a targeted approach, direct renin inhibitors promised precision. Despite early optimism, usage revealed inconsistent benefits and potential adverse effects. With ACE inhibitors and ARBs offering proven outcomes, direct renin inhibitors became less common in modern treatment.
Sodium Thiocyanate
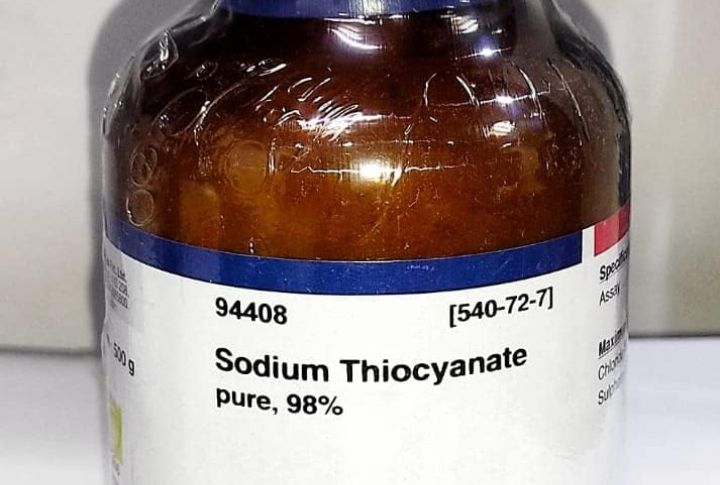
Sodium thiocyanate was among the first antihypertensive agents used clinically to relax the vascular smooth muscle and lower blood pressure. However, its high risk of hypothyroidism and cyanide accumulation led clinicians to abandon it in favor of newer drugs with wider safety margins.
Debrisoquine

Bruno Guerrero/Unsplash
Frequent reports of gastrointestinal upset and severe electrolyte imbalances overshadowed the early promise of debrisoquine, with more reliable antihypertensives being used now. First introduced in the 1950s to deplete catecholamines in peripheral sympathetic neurons and lower vascular tone, its unpredictable efficacy and safety concerns prompted doctors to abandon it.
Tolazoline

Tolazoline served as a nonselective alpha-adrenergic antagonist that produced peripheral vasodilation for lower blood pressure in resistant cases. Its therapeutic appeal declined after severe tachycardia and gastrointestinal upset emerged as common adverse effects. Moreover, the development of targeted alpha-blockers and calcium channel modulators has eliminated tolazoline from standard hypertension treatment.

